The rising rate of obesity in the United States is a growing concern for American healthcare. The prevalence of obesity from 2011-2014 among U.S. adults was estimated to be 36.5%, and epidemiologic studies have shown that obese individuals are at higher risk for developing metabolic and cardiovascular disease. Two possible explanations for this increased risk involve high-fat diet and release of free fatty acids from enlarged adipocytes (fat-storing cells), both of which increase the risk of atherosclerotic rupture and thrombosis.
The common thread in both explanations involves vascular inflammation. Traditionally we associate inflammation with the body’s immune system fighting off foreign bodies or pathogens, a state of illness. Thus, the presence of chronic inflammation in the walls of blood vessels during a state of obesity indicates that it is pathophysiologic.
To better understand the exact mechanism by which fatty acids cause inflammation, we studied a prominent mediator of vascular inflammation, cyclooxygenase-2 (COX-2) for my scholarly project. Under normal physiologic conditions, it is expressed minimally but can be induced in pathophysiologic conditions. The enzyme is responsible for downstream production of prostanoids including prostaglandin, prostacyclin, and thromboxane, all of which play a key role in vasoconstriction, vasodilation, platelet aggregation, and apoptosis.
COX-2 can be induced by cytokines from the body’s immune system or endotoxins from pathogens, activating a classical inflammatory pathway. However, newer research has demonstrated that free fatty acids can trigger the same inflammatory response in the absence of pathogens, termed “sterile inflammation.”
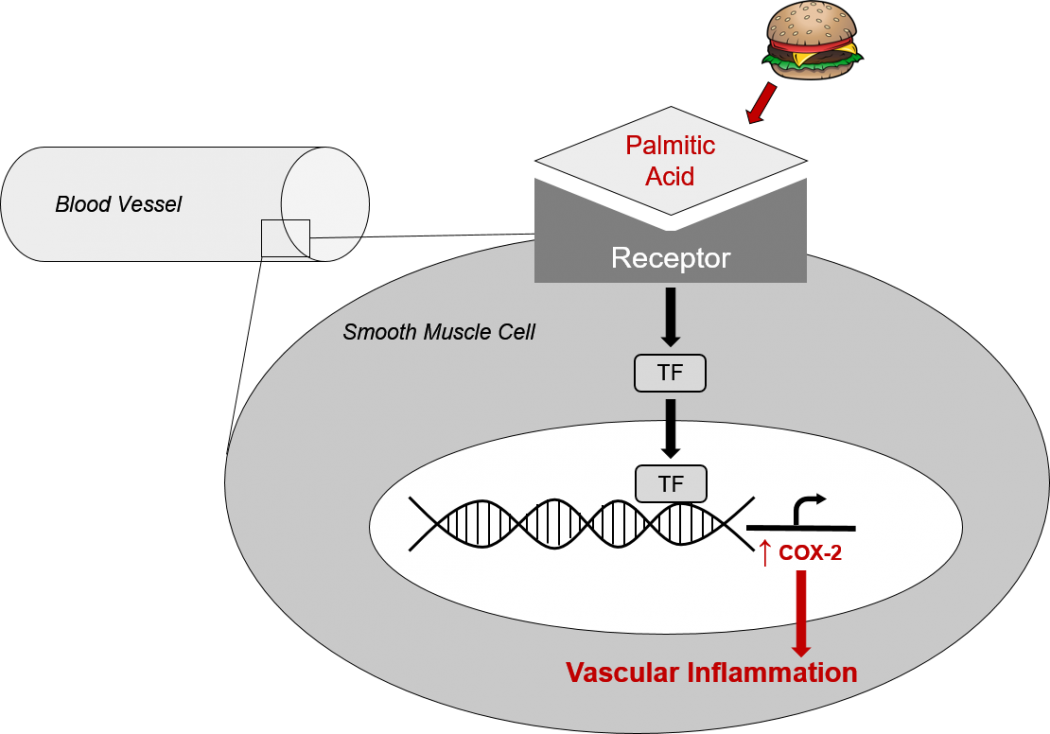
A cellular diagram of how palmitic acid, the most abundant dietary saturated fat, induces inflammation in the vessel wall. It binds a receptor on the surface of smooth muscle cells, activating a transcription factor which increases the amount of COX-2 protein. COX-2 then increases production of prostanoids, causing deleterious effects on blood vessel health.
The objective of our project is to characterize the mechanisms by which palmitic acid, the most abundant saturated fat, induces inflammation via COX-2 in the smooth muscle cells that line the walls of blood vessels. Our cell model uses primary human cells from a biotechnology company, Lonza. They receive donor tissue, harvest cells, and make them available for researchers who wish to conduct experiments with the highest physiological relevancy for in vitro tools. We purchased coronary artery smooth muscle cells of female human origin, cultured them for a minimal amount of passages, and treated with palmitate, the anion form of palmitic acid that occurs at physiologic pH. We used Western blot to evaluate the protein levels of COX-2 in those treated cells compared to a control group.
We found that palmitic acid increased total COX-2 protein and activity in these cells, measured by downstream prostaglandin production. Additionally, palmitic acid affected the glycosylation of COX-2, a method of post-translational modification that modulates the activity of COX-2. Palmitic acid increased the glycosylation of COX-2, which in turn increased the downstream prostaglandin production.
So what does this all mean, and where do we go from here? First, it means there are multiple mechanisms by which COX-2 causes vascular inflammation, some of which may be unique to the chronic saturated fatty acid exposure in obesity. Second, understanding these mechanisms may provide better therapeutic targets for preserving or restoring vascular function while treating patients for obesity and their related cardiovascular diseases.
My mentor, Dr. Rayna Gonzales, and I are hoping to further explore this topic as I continue my Scholarly Project. The SP program has refined my ability to develop a research question, to execute a plan for assessing that question, and to critically evaluate publications. I am confident that these skills will continue to serve me through my medical education and career as a physician.
- Ogden CL, Carroll MD, Fryar CD, Flegal KM. Prevalence of Obesity Among Adults and Youth: United States, 2011-2014. NCHS Data Brief. 2015;(219):1-8.
- Vaneckova I, Maletinska L, Behuliak M, Nagelova V, Zicha J, Kunes J. Obesity-related hypertension: possible pathophysiological mechanisms. J Endocrinol. 2014;223(3):R63-R78.
- Matsushima S, Kinugawa S, Yokota T, et al. Increased myocardial NAD(P)H oxidase-derived superoxide causes the exacerbation of postinfarct heart failure in type 2 diabetes. Am J Physiol Heart Circ Physiol. 2009;297(1):H409-16.
Puneet Raman is a second-year medical student at The University of Arizona College of Medicine – Phoenix. He attended Duke University where he received a Bachelor of Arts in history and a Bachelor of Science in biology. Puneet is passionate about using basic science research to lay the foundations for future clinical breakthroughs and hopes to continue to conduct research throughout his career in medicine. To contact Puneet, please e-mail him at puneetraman[at]email.arizona.edu.